By The Numbers: The Invisible Illness Care Journey
Anyone who lives with a complex, chronic disease is all too familiar with the ways that the healthcare system is not set up for us.
But not everyone is aware. With your help, we’re quantifying the ways that the system lets us down so that we can all advocate for better care.
The Healthcare System Fails Invisible Illness Patients
The long, windy, arduous path to a diagnosis (possibly with a misdiagnosis or two along the way). The myriad administrative tasks that we must shoulder as the quarterback of our care journey, from researching conditions to finding specialists to wrangling medical records to fighting with insurance. The provider who doesn’t quite believe us when we talk about what we’re going through, when we say we know that something is wrong. Who ascribes our symptoms to anxiety, or maybe to our weight.
The way it all can make us feel like our plight is as invisible as some of our symptoms.
At Chronius, we see you. We hear you. Even when the healthcare system doesn’t.
That’s why we have started surveying patients to put quantitative backing behind many of the challenges that we face when navigating the healthcare system. Numbers don’t lie, and the numbers show undeniably that the system is broken.
Because many complex, chronic conditions are invisible and under-researched, most people - even doctors! - don't really understand how difficult it is to become diagnosed for and manage a complex, chronic disease. The goal for this report is to paint a picture of what patients must go through so that:
Stakeholders in the healthcare system can better understand how invisible illness patients are let down by the system
Advocates fighting for more research dollars for woefully underfunded conditions can have robust quantitative ammunition in their fight
Would-be allies - like friends and family and coworkers - can have a deeper understanding of what we go through
Though our survey size so far is small (n=~100), we hope to grow the respondent base over time with your help. You can contribute the high-level details of your care journey here (your answers will be completely anonymized). And feel free to share the survey far and wide with relevant individuals!
Read on to learn more about the care journeys of people who live with complex, chronic illnesses. If you’d like to share more qualitative details of your care journey experience, or share your thoughts in general about the survey and survey results, you can reach us at info@chroniushealth.com.
Getting To A Diagnosis
The luckiest among us are diagnosed within a year or two of first experiencing symptoms. But this is not the experience of most. In fact, our research shows that it takes, on average, 6.8 years to reach a diagnosis for a complex, chronic condition (3.0 years is the median). And the average obscures the fact that for many, it can take literally decades to get diagnosed: one respondent’s diagnosis journey was 36 years.
And the diagnosis journey is not exactly a walk in the park. It’s more like a constant struggle.
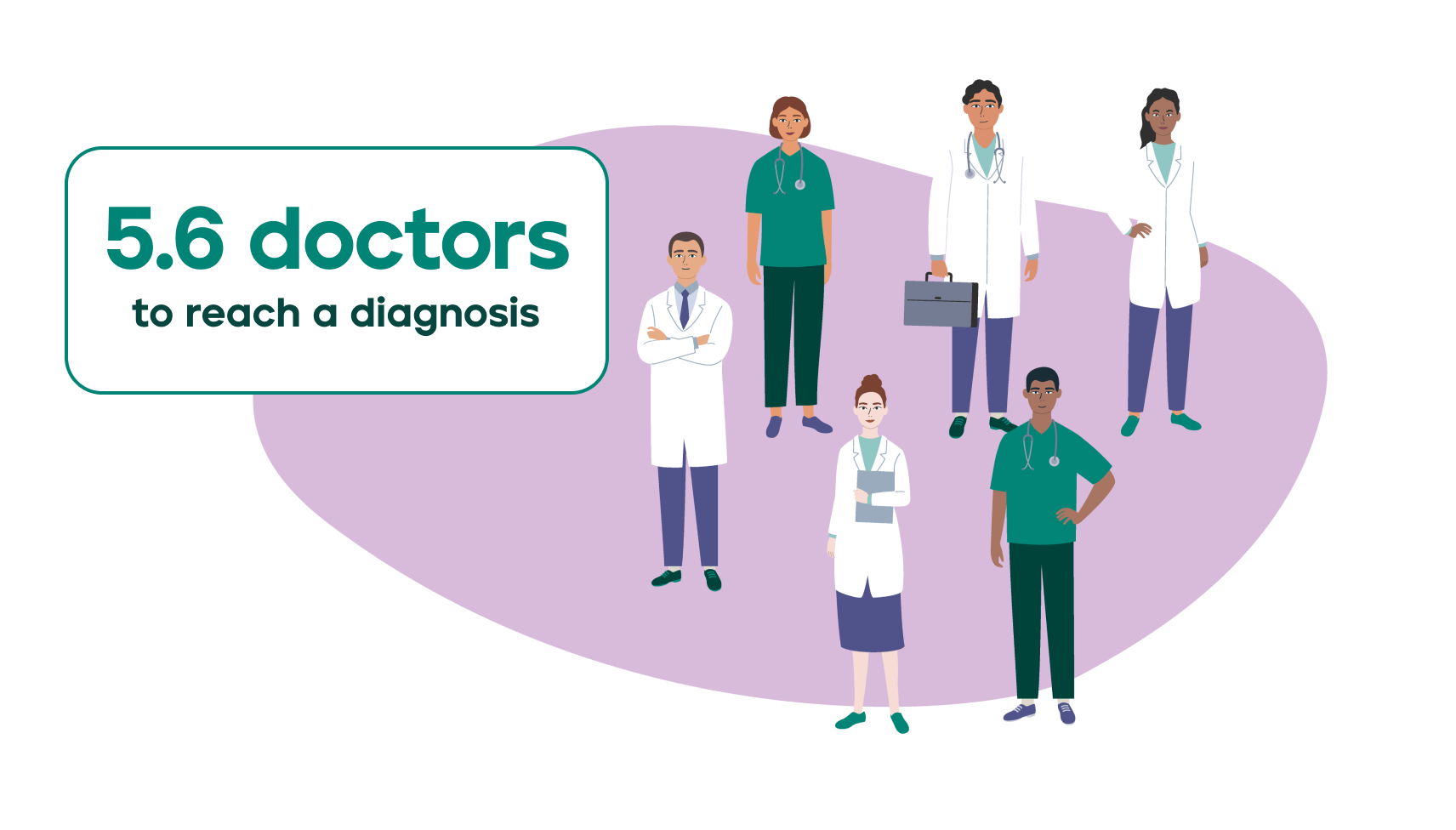
In part, this is due to the unrelenting administrative burden that patients must shoulder as the quarterback of their care. For example, patients report spending 42 hours conducting research on their symptoms and potential diagnoses. Not to mention the litany of tests patients must undergo and specialists they must see. While seeking a diagnosis, patients can expect to see 5.6 different doctors (with some needing to see as many as 20), possibly multiple times each. Most complex, chronic conditions - which usually do not have a clear biomarker to definitively signal their presence - are what is called a “diagnosis of exclusion”. This means patients must patiently wait as many other conditions are first ruled out before their final, formal diagnosis can be declared.
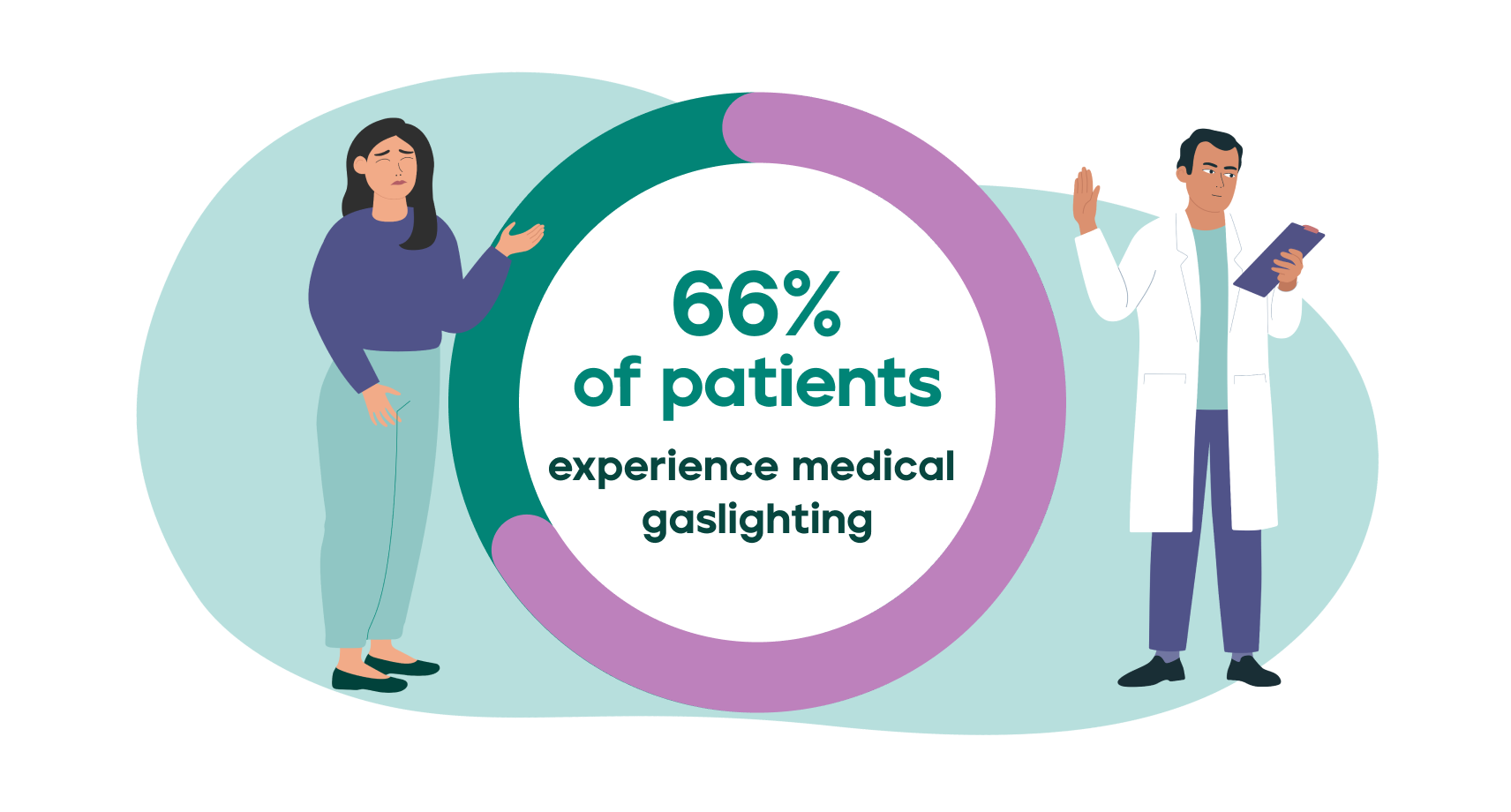
But much of the burden comes from completely unnecessary - and downright unjust - hurdles and stressors patients face. Increasingly, patients are speaking up about “medical gaslighting”, or the experience of having a medical professional dismiss, ignore, or trivialize a patient’s legitimate health concerns. An astounding 66% of patients experience medical gaslighting during their diagnosis journey. Specifically, 45% had their symptoms attributed primarily to a mental health condition such as anxiety, depression, or stress, and 43% had their symptoms attributed primarily to their being “overweight”.
This is, of course, entirely unacceptable, and many patients refuse to accept it: 54% switch providers to find one who takes their concerns seriously. Failing to take patients’ testimony seriously leads to far too many misdiagnoses, with patients misdiagnosed 1.5 times, on average. Providers who do not adequately listen to a patient’s history, or who do listen but aren’t set up to coordinate effectively with other providers that comprise a patient’s extended care team, often end up putting their patients through unnecessary, redundant tests. To reach a diagnosis, patients undergo 1.0 redundant procedures.
Over and above all of the avoidable pain, anguish, and stress that these challenges cause for patients is the cardinal sin of the healthcare system: wasted, inefficient spending. A patient that takes 8.6 years to reach a diagnosis - before even beginning their treatment regimen! - all while churning through providers and suffering through redundant tests is a very expensive patient indeed.
Managing An Invisible Illness
The care journey is just beginning once we reach a formal diagnosis. Chronic conditions are… chronic, after all. The burden of being a patient never relents.
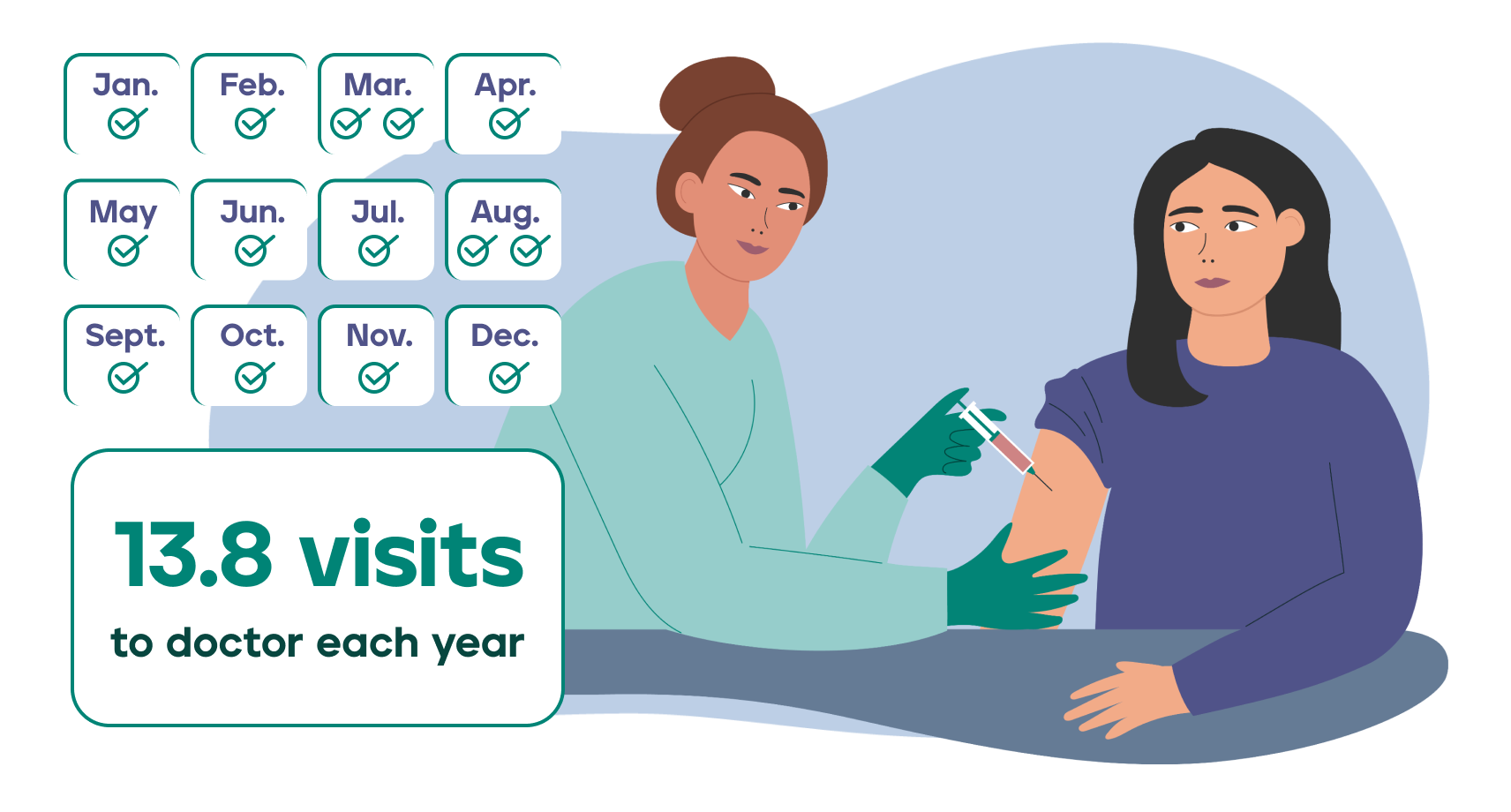
Patients have, on average, 13.8 doctor visits each year. Only 50% of patients say their providers have a “robust” or “expert” understanding of their condition and can be frequently helpful. So more than 1 appointment per month, only half of which are helpful…
Acute, emergency visits are common for patients managing a complex, chronic condition. Patients with invisible illness visit the ED 1.4 times per year and visit Urgent Care 1.0 times per year.
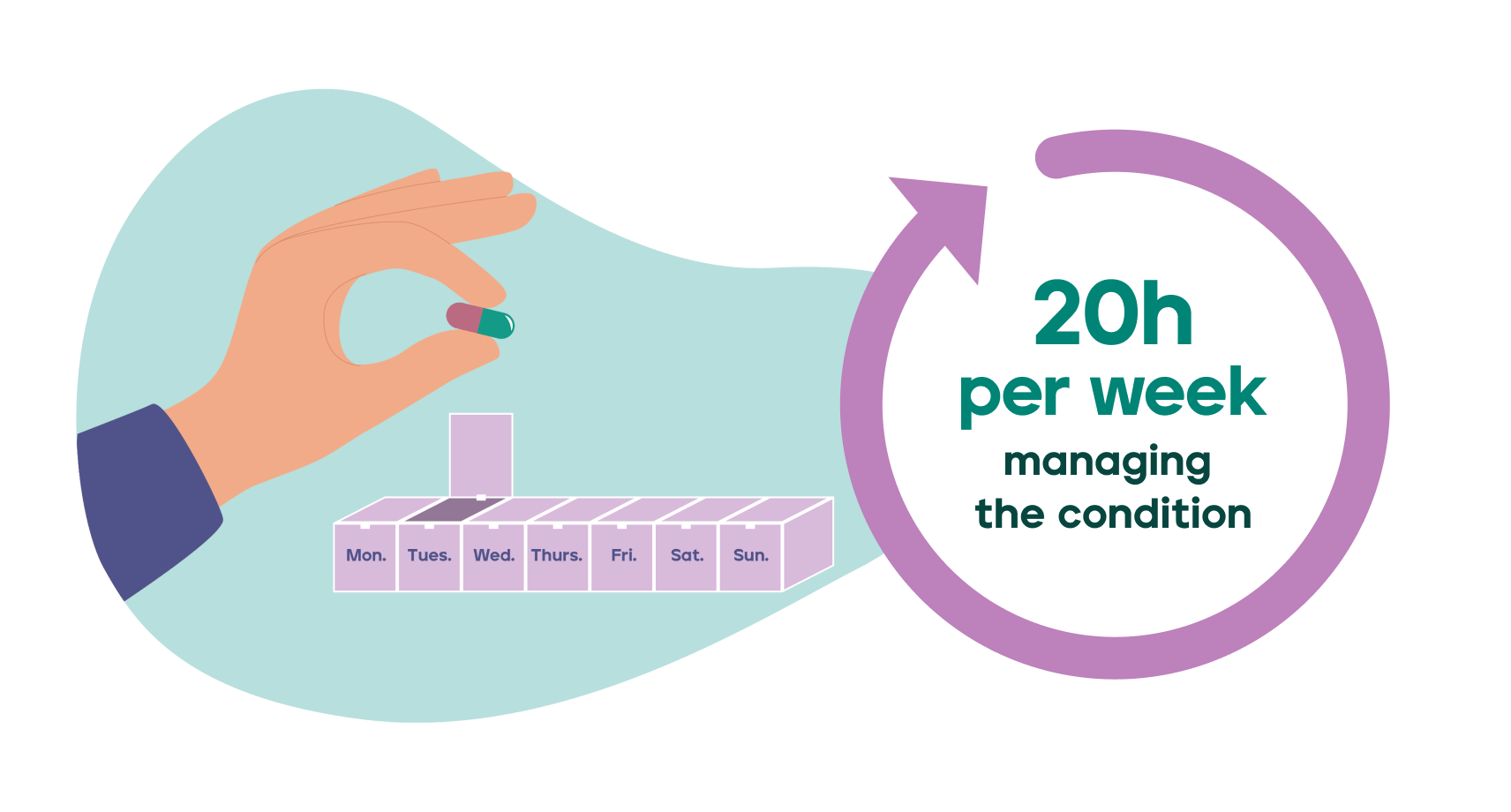
Accordingly, the time we spend just managing everything related to our condition is significant. Patients spend a whopping 20 hours per week managing their condition. Just preparing for an appointment takes 4.6 hours, on average. Maintaining our status quo is exhausting, and can come to feel like an unpaid, un-asked-for, full-time job.
This is all before considering the fact that many of us end up juggling multiple conditions. The average patient with a complex, chronic condition actually has 2.2 complex, chronic conditions; 32% are polychronic (2 or more complex, chronic conditions). If new symptoms set us on a path to another diagnosis, we have to figure out how to navigate that difficult diagnosis journey (again!) while simultaneously managing everything that comes along with our first (or second, or third…) condition. The second diagnosis journey might even be more difficult than the first because symptoms can overlap between conditions, making diagnosis even more challenging than usual.
It Shouldn’t Be So Hard To Have An Invisible Illness
Patients shouldn’t have to manage all of this and also be responsible for driving the advocacy that will change the system for the better. But just as we are our own best advocates in the doctor’s office, so too are we our own best advocates when pushing for better treatment by the system at large.
We refuse to accept the healthcare system as it is. We firmly believe that invisible illness patients deserve better. And we know that we can get better treatment, and that we ultimately will.
Until then, we need to continue advocating for change and spreading awareness of what it is like to live with a complex, chronic condition. Hopefully the cold, hard facts in this report makes that advocacy just a little bit easier.
To download a PDF infographic of the results of our survey, click here.